Strong RSV vaccine data lifts hopes after years of futility
New research shows vaccinating pregnant women helped protect their newborns from the common but scary respiratory virus called RSV that fills hospitals with wheezing babies each fall. The preliminary results buoy hope that after decades of failure and frustration, vaccines against RSV may finally be getting close...
New research shows vaccinating pregnant women helped protect their newborns from the common but scary respiratory virus called RSV that fills hospitals with wheezing babies each fall.
The preliminary results buoy hope that after decades of failure and frustration, vaccines against RSV may finally be getting close.
Pfizer announced Tuesday that a large international study found vaccinating moms-to-be was nearly 82% effective at preventing severe cases of RSV in their babies' most vulnerable first 90 days of life. At age 6 months, the vaccine still was proving 69% effective against serious illness -- and there were no signs of safety problems in mothers or babies.
"Moms are always giving their antibodies to their baby," said virologist Kena Swanson, Pfizer's vice president of viral vaccines. "The vaccine just puts them in that much better position" to form and pass on RSV-fighting antibodies.
The vaccine quest isn't just to protect infants. RSV is dangerous for older adults, too, and both Pfizer and rival GSK recently announced that their competing shots also proved protective for seniors.
None of the findings will help this year when an early RSV surge already is crowding children's hospitals. But they raise the prospect that one or more vaccines might become available before next fall's RSV season.
"My fingers are crossed," said Dr. William Schaffner, an infectious disease specialist at Vanderbilt University. "We're making inroads."
Tuesday's data was reported in a press release and hasn't been vetted by independent experts.
Here's a look at the long quest for RSV vaccines.
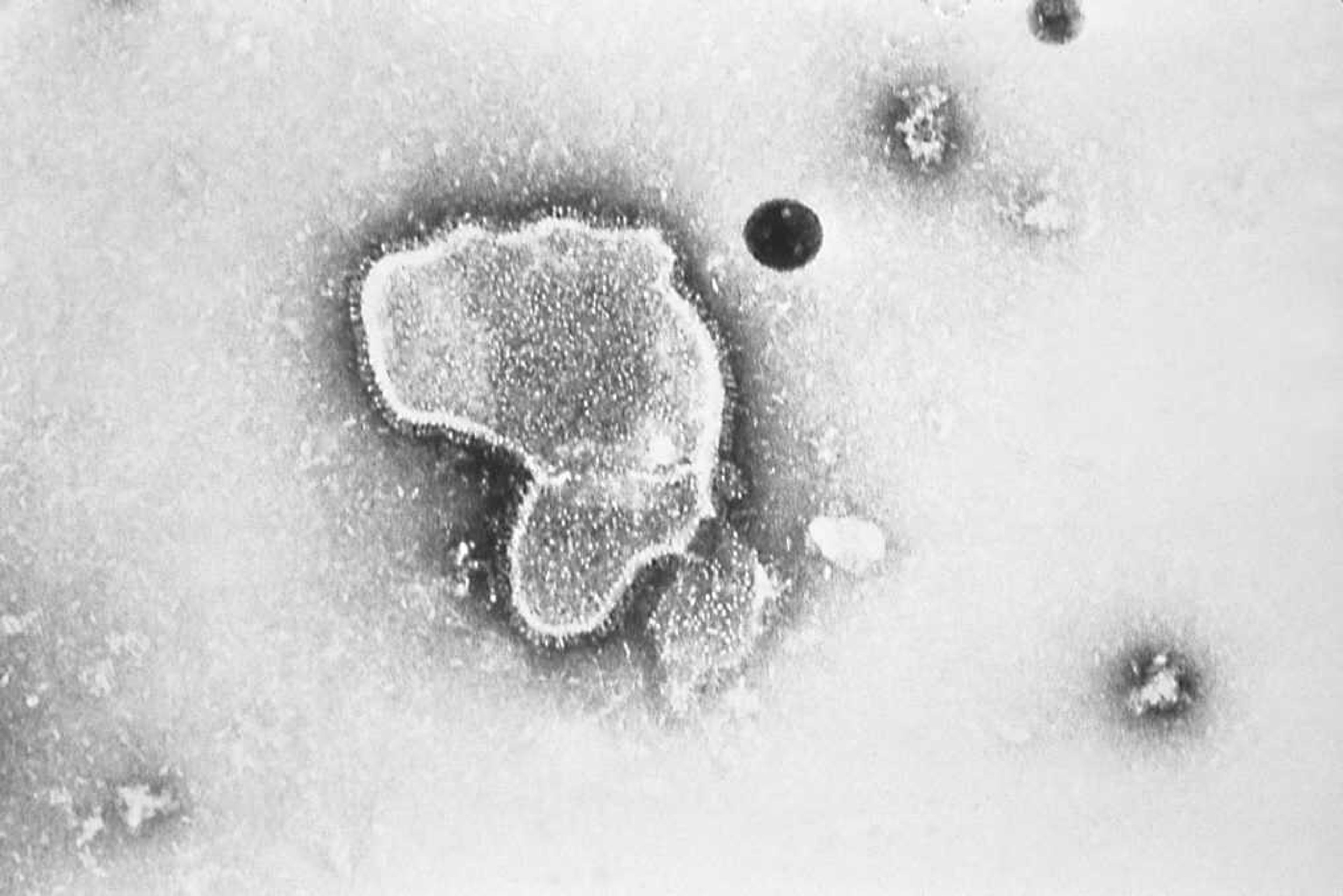
What is RSV?
For most healthy people, RSV, or respiratory syncytial virus, is a cold-like nuisance. But for the very young, the elderly and people with certain health problems, it can be serious, even life-threatening. The virus can infect deep in the lungs, causing pneumonia, and in babies it can impede breathing by inflaming tiny airways.
In the U.S., about 58,000 children younger than 5 are hospitalized for RSV each year and several hundred die. Among adults 65 and older, about 177,000 are hospitalized with RSV and 14,000 die annually.
Worldwide, RSV kills about 100,000 children a year, mostly in poor countries.
Why is there no vaccine?
A tragedy in the 1960s set back the whole field. Using the approach that led to the first polio vaccine, scientists made an experimental RSV vaccine by growing the virus in a lab and killing it. But testing in children found not only was the vaccine not protective, youngsters who caught RSV after vaccination fared worse. Two died.
"For a period of 20 years, even though science was advancing, nobody wanted to go near development of an RSV vaccine," Schaffner said.
Even today's modern RSV vaccine candidates were tested first in older adults, not children, he noted.
What got development back on track?
Modern vaccines tend to target the outer surface of a virus, what the immune system sees when a germ invades. For RSV, that target is the so-called F protein that helps the virus latch onto human cells. Again there was a hurdle: That protein is a shape-shifter, rearranging its form before and after it "fuses" to cells.
It turns out that the immune system only forms effective RSV-fighting antibodies when it spots what's called the pre-fusion version of that protein, explained structural biologist Jason McLellan of the University of Texas at Austin.
In 2013, McLellan and virologist Barney Graham were working at the National Institutes of Health when they homed in on the correct shape and figured out how to freeze it in that form. That finding opened the way to today's development of a variety of experimental RSV vaccine candidates.
(That same discovery was key to the hugely successful COVID-19 vaccines, as the coronavirus also is cloaked in a shape-shifting surface protein.)
What's in the pipeline?
Several companies are creating RSV vaccines but Pfizer and rival GSK are furthest along. Both companies recently reported final-stage testing in older adults. The competing vaccines are made somewhat differently but each proved strongly effective, especially against serious disease. Both companies plan to seek regulatory approval in the U.S. by the end of the year, as well as in other countries.
The older-adult data "looks fantastic," said McLellan, who has closely followed the vaccine development. "I think we're on the right track."
And if vaccinating pregnant women pans out, it could be "a win for two individuals instead of just one," by offering protection to both mom-to-be and baby, said Dr. Wilbur Chen of the University of Maryland School of Medicine.
Pfizer's maternal vaccine is the same recipe that it tested successfully in older adults -- and it also plans to seek Food and Drug Administration approval for those vaccinations by year's end.
The new study included 7,400 pregnant women in 18 countries, including the U.S., and spanned multiple RSV seasons. Preliminary results reported Tuesday show the vaccine was most effective against severe disease. For milder illness, effectiveness was 51% to 57% -- short of the study's statistical requirements but a result that Pfizer still called clinically meaningful because it could mean fewer trips to the doctor's office.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute's Department of Science Education. The AP is solely responsible for all content.
Connect with the Southeast Missourian Newsroom:
For corrections to this story or other insights for the editor, click here. To submit a letter to the editor, click here. To learn about the Southeast Missourian’s AI Policy, click here.