More to explore
-
 Local News 5/20/24Two shot at Cape Central graduation ceremony; one suspect in custody8One person was in custody after a shooting at Cape Central High School’s graduation ceremony left two people injured Sunday, May 19. According to Cape Girardeau Police Department, an altercation between two people during the event at the Show Me...
Local News 5/20/24Two shot at Cape Central graduation ceremony; one suspect in custody8One person was in custody after a shooting at Cape Central High School’s graduation ceremony left two people injured Sunday, May 19. According to Cape Girardeau Police Department, an altercation between two people during the event at the Show Me... -
 Local News 5/20/24Mother’s Day stray dog attack in Scott County raises questions about local animal controlOn Mother’s Day morning, Sandy Ruff noticed a stray dog near her home. Believing it to have been abandoned in the area by its owner, Ruff took a photo of the dog and posted it to Facebook, looking for its owner or someone to take it in. According to...
Local News 5/20/24Mother’s Day stray dog attack in Scott County raises questions about local animal controlOn Mother’s Day morning, Sandy Ruff noticed a stray dog near her home. Believing it to have been abandoned in the area by its owner, Ruff took a photo of the dog and posted it to Facebook, looking for its owner or someone to take it in. According to... -

-
 Local News 5/19/24Cape Girardeau Public Schools issues statement following shooting at graduation ceremony3Cape Girardeau Public Schools superintendent Howard Benyon issued a statement Sunday afternoon, May 19, following a shooting during the district's high school graduation that left at least one person injured. "During our graduation ceremony today at...
Local News 5/19/24Cape Girardeau Public Schools issues statement following shooting at graduation ceremony3Cape Girardeau Public Schools superintendent Howard Benyon issued a statement Sunday afternoon, May 19, following a shooting during the district's high school graduation that left at least one person injured. "During our graduation ceremony today at... -
 Local News 5/19/24Two shot at Cape Central graduation ceremony3One person was shot at Cape Girardeau Central High School's graduation ceremony Sunday, May 19. A Black male was shot in the leg in the concession area on the second floor of the Show Me Center on the campus of Southeast Missouri State University....
Local News 5/19/24Two shot at Cape Central graduation ceremony3One person was shot at Cape Girardeau Central High School's graduation ceremony Sunday, May 19. A Black male was shot in the leg in the concession area on the second floor of the Show Me Center on the campus of Southeast Missouri State University.... -

-
 Local News 5/19/24Police chief says two may have been injured at Cape Central graduationCape Girardeau police chief Wes Blair said two people may have been shot at Cape Girardeau Central High School's graduation ceremony Sunday, May 19, at the Show Me Center on the campus of Southeast Missouri State University. Shortly after 4 p.m.,...
Local News 5/19/24Police chief says two may have been injured at Cape Central graduationCape Girardeau police chief Wes Blair said two people may have been shot at Cape Girardeau Central High School's graduation ceremony Sunday, May 19, at the Show Me Center on the campus of Southeast Missouri State University. Shortly after 4 p.m.,... -
 Local News 5/19/24One shot at Cape Central graduationOne person was shot at Cape Girardeau Central High School's graduation ceremony. A Southeast Missourian reporter at the scene said one person had been shot in the leg. The incident occurred about 2:30 p.m. This breaking news will be updated as...
Local News 5/19/24One shot at Cape Central graduationOne person was shot at Cape Girardeau Central High School's graduation ceremony. A Southeast Missourian reporter at the scene said one person had been shot in the leg. The incident occurred about 2:30 p.m. This breaking news will be updated as... -

-
 Local News 5/18/24Signs of summer
Local News 5/18/24Signs of summer -
 Photo Gallery 5/18/24Jackson Graduation 2024
Photo Gallery 5/18/24Jackson Graduation 2024 -
 Local News 5/18/24Seventh annual Dancing with Show Me Stars to feature new silent auctionThe seventh annual Dancing with Show Me Stars will feature a silent auction for the first time in the event’s history. The “Heroes vs. Villains”-themed gala will start at 7 p.m. June 29 with doors opening at the Show Me Center at 6 p.m. The event...
Local News 5/18/24Seventh annual Dancing with Show Me Stars to feature new silent auctionThe seventh annual Dancing with Show Me Stars will feature a silent auction for the first time in the event’s history. The “Heroes vs. Villains”-themed gala will start at 7 p.m. June 29 with doors opening at the Show Me Center at 6 p.m. The event... -

-
 Local News 5/17/24SEMO, Cape Central graduate selected for prestigious law program8A Southeast Missouri State University graduate is one of the newest recipients of a prominent scholarship geared toward those planning to practice civil rights law in the South. Miracle Bird, who received her master’s degree from the university on...
Local News 5/17/24SEMO, Cape Central graduate selected for prestigious law program8A Southeast Missouri State University graduate is one of the newest recipients of a prominent scholarship geared toward those planning to practice civil rights law in the South. Miracle Bird, who received her master’s degree from the university on... -
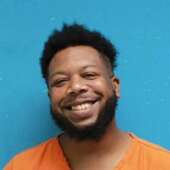
 Local News 5/17/24Scott City Police say St. Louis man on probation for robbery possessed weapon illegallyA St. Louis man is in jail in lieu of a $50,000 cash/surety bond for a weapons case in Scott City. Tyreece Martin was arrested after Scott City officers responded to a call that an armed man refused to leave a residence, a news release issued by the...
Local News 5/17/24Scott City Police say St. Louis man on probation for robbery possessed weapon illegallyA St. Louis man is in jail in lieu of a $50,000 cash/surety bond for a weapons case in Scott City. Tyreece Martin was arrested after Scott City officers responded to a call that an armed man refused to leave a residence, a news release issued by the... -
 Local News 5/17/24Central Academy's MO-Ops students post 100% passing rate on high school equivalency exams6For the first time in the school's history, Cape Central Academy's Missouri Option Program (MO-Ops) students posted a 100% passing rate on the HISET exams, allowing all 13 students enrolled in the program to earn their high school diplomas. Cape...
Local News 5/17/24Central Academy's MO-Ops students post 100% passing rate on high school equivalency exams6For the first time in the school's history, Cape Central Academy's Missouri Option Program (MO-Ops) students posted a 100% passing rate on the HISET exams, allowing all 13 students enrolled in the program to earn their high school diplomas. Cape... -

-
 Local News 5/17/24Several city streets to be under under construction in the next week3The City of Cape Girardeau updated what street work will continue or start in the next week with Perryville Road and Lexington Avenue. According to an email, work on Perryville Road will start as soon as May 20 to 24 on Cape Rock Drive and will run...
Local News 5/17/24Several city streets to be under under construction in the next week3The City of Cape Girardeau updated what street work will continue or start in the next week with Perryville Road and Lexington Avenue. According to an email, work on Perryville Road will start as soon as May 20 to 24 on Cape Rock Drive and will run... -

-
 Local News 5/16/24Scout Hall's Next Act: EXP ShowcaseFive local artists will be putting their talents on display at the EXP Showcase at Scout Hall on Friday, May 17. EXP Productions is a collaboration of musicians and songwriters from the region who have come together not only to help each other...
Local News 5/16/24Scout Hall's Next Act: EXP ShowcaseFive local artists will be putting their talents on display at the EXP Showcase at Scout Hall on Friday, May 17. EXP Productions is a collaboration of musicians and songwriters from the region who have come together not only to help each other... -
 Local News 5/16/24Jordan asks for another extension in civil case to remove the coroner from office15Cape Girardeau Coroner Wavis Jordan has asked for another 30-day extension as he tries to find an attorney to represent him in the civil case filed by the Missouri Attorney General’s Office. The state’s filing seeks to remove Jordan from his post....
Local News 5/16/24Jordan asks for another extension in civil case to remove the coroner from office15Cape Girardeau Coroner Wavis Jordan has asked for another 30-day extension as he tries to find an attorney to represent him in the civil case filed by the Missouri Attorney General’s Office. The state’s filing seeks to remove Jordan from his post.... -
 Local News 5/16/24James Clay Waller III faces domestic assault charge; victim claims he was knocked unconscious4James Clay Waller III, 32, of Jackson, has been charged with third-degree assault on allegations he lured a man to a location and injured the victim in a fight. The victim told police on May 5 that Waller sent the victim text messages while...
Local News 5/16/24James Clay Waller III faces domestic assault charge; victim claims he was knocked unconscious4James Clay Waller III, 32, of Jackson, has been charged with third-degree assault on allegations he lured a man to a location and injured the victim in a fight. The victim told police on May 5 that Waller sent the victim text messages while... -
 Local News 5/16/24Cape man arrested on allegations he fired a gun while intoxicated1While investigating a shots fired call, police say they found an intoxicated Cape Girardeau man who fired his weapon five times while walking near an apartment complex. Christian Cole, 34, faces the Class E felony charge of unlawful use of a weapon...
Local News 5/16/24Cape man arrested on allegations he fired a gun while intoxicated1While investigating a shots fired call, police say they found an intoxicated Cape Girardeau man who fired his weapon five times while walking near an apartment complex. Christian Cole, 34, faces the Class E felony charge of unlawful use of a weapon... -
 Local News 5/16/24SEMO relaunches online MBA degree to include students without undergrad business degrees3Southeast Missouri State University announced the relaunch of its online Master of Business Administration (MBA) general management degree on Monday, allowing students to enroll in the program even if they don't have an undergraduate business...
Local News 5/16/24SEMO relaunches online MBA degree to include students without undergrad business degrees3Southeast Missouri State University announced the relaunch of its online Master of Business Administration (MBA) general management degree on Monday, allowing students to enroll in the program even if they don't have an undergraduate business... -

-

-
 Local News 5/16/24County Road 413 in Scott County closed for culvert replacementCounty Road 413 in Scott County will be closed as Missouri Department of Transportation crews replace a culvert under the roadway, according to a MoDOT news release. This section of road is at the junction of Route W and County Road 413 near Oran....
Local News 5/16/24County Road 413 in Scott County closed for culvert replacementCounty Road 413 in Scott County will be closed as Missouri Department of Transportation crews replace a culvert under the roadway, according to a MoDOT news release. This section of road is at the junction of Route W and County Road 413 near Oran.... -
 Photo Gallery 5/16/24Chaffee Graduation 2024
Photo Gallery 5/16/24Chaffee Graduation 2024 -

-
 Most read 5/15/24Cost savings appear at heart of potential contract change between City, Chamber5The City of Cape Girardeau could save $164,327 annually by merging Visit Cape and the municipal Parks and Recreation Department, according to a proposal obtained by the Southeast Missourian. The proposal, put forth by the city’s Parks and Recreation...
Most read 5/15/24Cost savings appear at heart of potential contract change between City, Chamber5The City of Cape Girardeau could save $164,327 annually by merging Visit Cape and the municipal Parks and Recreation Department, according to a proposal obtained by the Southeast Missourian. The proposal, put forth by the city’s Parks and Recreation... -
 Most read 5/15/24Woman sets up donation drive for cat that needs leg amputated after being shot in Cape neighborhood5A Cape Girardeau woman has set up a fundraiser to get care for a neighborhood cat she named Garfield, who she says was shot in the leg. Madelyn Bandermann took to social media to share that an outside cat that she feeds and cares for was missing for...
Most read 5/15/24Woman sets up donation drive for cat that needs leg amputated after being shot in Cape neighborhood5A Cape Girardeau woman has set up a fundraiser to get care for a neighborhood cat she named Garfield, who she says was shot in the leg. Madelyn Bandermann took to social media to share that an outside cat that she feeds and cares for was missing for... -
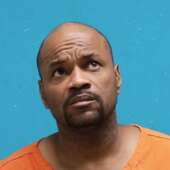
 Most read 5/14/24Cape Girardeau County coroner waives hearing in criminal case9Cape Girardeau County Coroner Wavis Jordan waived a preliminary hearing in his ongoing criminal case in Cape Girardeau County Court on Tuesday, May 14. A preliminary hearing is a standard practice for the prosecution to give evidence to convince a...
Most read 5/14/24Cape Girardeau County coroner waives hearing in criminal case9Cape Girardeau County Coroner Wavis Jordan waived a preliminary hearing in his ongoing criminal case in Cape Girardeau County Court on Tuesday, May 14. A preliminary hearing is a standard practice for the prosecution to give evidence to convince a... -
 Most read 5/14/24Jackson man faces charges after allegedly threatening to kill victim, burn house downA Jackson man is in jail after a victim told police he threatened to kill her and burn down the house after previous reports of abuse. Bradley J. Moreland, 41, faces Class E felony charges of third-degree domestic assault and first-degree...
Most read 5/14/24Jackson man faces charges after allegedly threatening to kill victim, burn house downA Jackson man is in jail after a victim told police he threatened to kill her and burn down the house after previous reports of abuse. Bradley J. Moreland, 41, faces Class E felony charges of third-degree domestic assault and first-degree... -
 Most read 5/14/24Sex offender arrested on allegations of repeatedly approaching children at Cape Girardeau park2A convicted sex offender living in Cape Girardeau is in jail in lieu of $25,000 cash-only bond after being accused of approaching children at a park. Cape Girardeau Police officers responded to a call on Sunday, May 12 from parents concerned that...
Most read 5/14/24Sex offender arrested on allegations of repeatedly approaching children at Cape Girardeau park2A convicted sex offender living in Cape Girardeau is in jail in lieu of $25,000 cash-only bond after being accused of approaching children at a park. Cape Girardeau Police officers responded to a call on Sunday, May 12 from parents concerned that... -
 Most read 5/13/24Ex-Sikeston cop receives 20-year sentence for child sexual abuse charges2A former Sikeston, Missouri, police officer was sentenced to 20 years in the Missouri Department of Corrections after his conviction of statutory rape of a child younger than than 14 years old. Brian L. Robinson was sentenced on May 3 to 20 years on...
Most read 5/13/24Ex-Sikeston cop receives 20-year sentence for child sexual abuse charges2A former Sikeston, Missouri, police officer was sentenced to 20 years in the Missouri Department of Corrections after his conviction of statutory rape of a child younger than than 14 years old. Brian L. Robinson was sentenced on May 3 to 20 years on... -
 Most read 5/13/24County commissioners updated on renovations for Melaina's Magical Playland2Melaina’s Magical Playland will be undergoing some renovations in the near future. During the Monday, May 13, meeting of the Cape Girardeau County Commission, the county’s park superintendent, Bryan Sander, notified the commissioners about replacing...
Most read 5/13/24County commissioners updated on renovations for Melaina's Magical Playland2Melaina’s Magical Playland will be undergoing some renovations in the near future. During the Monday, May 13, meeting of the Cape Girardeau County Commission, the county’s park superintendent, Bryan Sander, notified the commissioners about replacing...

Respond to this story
Posting a comment requires a subscription.